Study in mice suggests genetic changes targeting macrophages may help
In recent years, a growing body of research has shown that the body can remember the pain of newborn injuries, including life-saving surgeries well into adolescence.
These early experiences appear to change the way children’s pain response systems develop at a genetic level, leading to more intense responses to pain later in life. This change also appears to be more common in women.
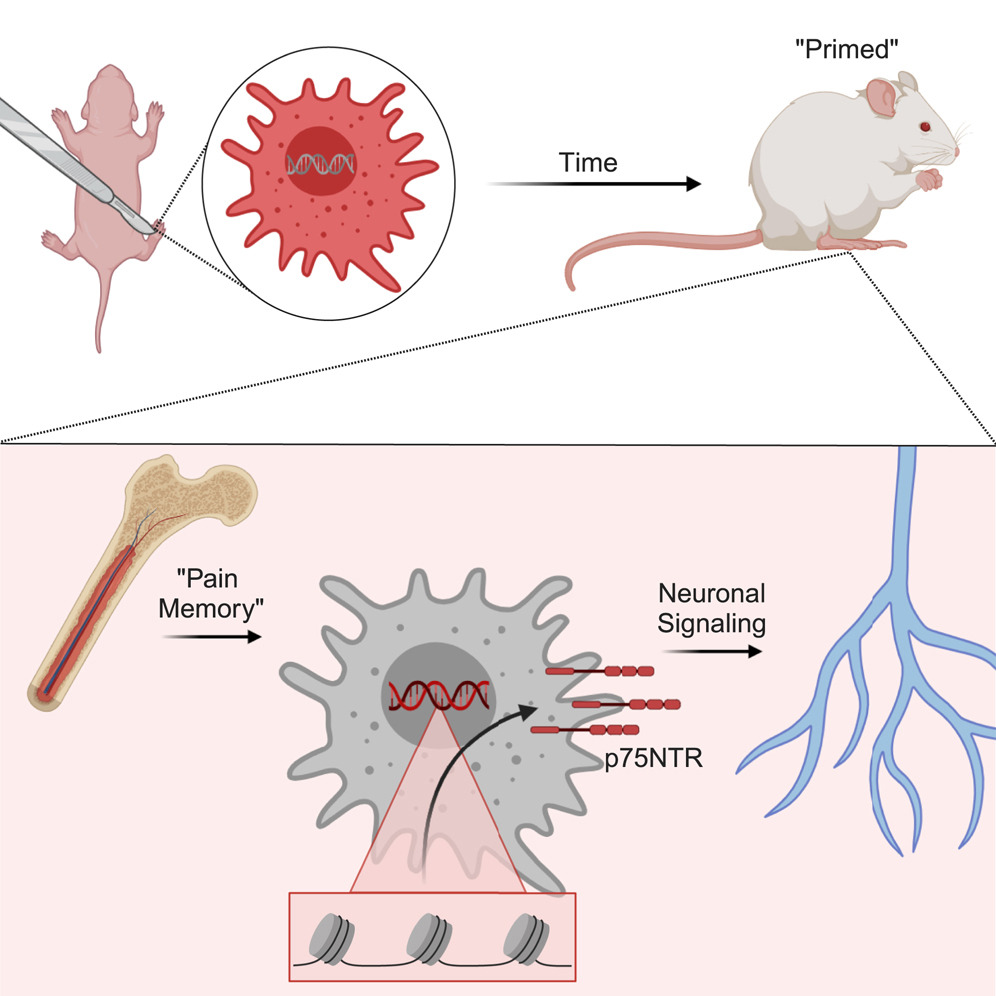
Now, research led by experts at Cincinnati Children’s Hospital has pinpointed how and where the genetic changes that create this lasting memory of pain occur.According to their research, published online on April 18, 2024 in the journal cell reportkey changes occur during the development of macrophages, a major component of the immune system.
Our experiments help further confirm how pain memories affect female newborns over longer periods of time. Specifically, our data show that epigenetic changes (changes that occur after birth versus inherited genetic variants) occur in macrophages after injury early in life, which in turn promotes responses to changes that occur later in life. Other injuries have a more intense pain response, said corresponding author Michael Jankowski, MD, associate director of the Center for Pediatric Pain Research at Cincinnati Children’s Hospital.
Dr. Adam Dourson is the study’s lead author and is currently at Washington University in St. Louis.
Experiments showed that male mice that experienced similar early-life insults showed the same epigenetic changes but did not maintain the same long-term pain memory as females.Further testing also showed that the change occurred in a file called p75NTRcan be found in human macrophages.
In female mice, pain memory effects were detected for more than 100 days after the initial injury. The incision causes stem cells in the bone marrow to produce macrophages, which respond more strongly to the injury, increasing pain.
For humans, a similar time frame is about 10 to 15 years.
“We were surprised how a single local injury could so dramatically alter the epigenetic/transcriptomic landscape of systemic macrophages,” Jankowski said.
This new understanding of neonatal pain memory highlights fundamental differences between the genetic activity of the still-developing neonatal immune system and the mature system of adults. This means determining how surgeons and care teams adapt rehabilitative care for newborns and baby girls will be complex.
Simply changing the pain medication dose may not be the answer. There is always a balance between controlling pain and minimizing possible harmful side effects of existing medications. Instead, our findings suggest the need to develop more specific, targeted treatments to prevent macrophages from reprogramming in response to injury, Jankowski said.
Next step
More research is needed to use this new information to develop therapies to control immune pain memory.
In this study, blocking the p75NTR receptor in young mice indeed impaired the ability of macrophages to communicate with sensory neurons and partially prevented prolonged pain-like behavior. However, it is unclear whether a similar approach can be safely used to target human macrophages.
Jankowski said the emerging technology appears to be able to specifically block the p75NTR receptor in macrophages, but much more research is needed before this approach is ready for human clinical trials.
About the study
In addition to Dourson and Jankowski, Cincinnati Children’s co-authors include Adewale Fadaka, Anna Warshak, Luis Queme and Megan Hofmann, Department of Anesthesiology; Aditi Paranjpe, Department of Bioinformatics; Benjamin Weinhaus and Daniel Daniel Lucas, Division of Experimental Hematology and Cancer Biology; Heather Evans and George Deepe, Jr., Division of Infectious Diseases; and Omer Donmez, Carmy Forney, Matthew Weirauch and Leah Kottyan, Center for Autoimmune Genomics and Etiology.
Experimental work for this study included support from the Flow Cytometry Core, Bioimaging and Analysis Facility, Center for Autoimmune Genomics and Etiology, and Cincinnati Children’s Hospital Comprehensive Mouse and Cancer Core.
Funding for this research included multiple grants from the National Institutes of Health (R01NS105715, R01NS113965, F31NS122494, R01HL160614, P30 AR070549; an ARC award from Cincinnati Children’s; and support from the Leukemia and Lymphoma Society.
#Immune #cells #lasting #memory #early #pain #Research #Horizons
Image Source : scienceblog.cincinnatichildrens.org